Attention Deficit Hyperactivity Disorder (ADHD) is a multifaceted neurodevelopmental condition that often impersonates the symptoms of other mental health issues, such as anxiety, depression, and mood dysregulation. ADHD is defined by behavioral symptoms like impulsivity, inattention, and hyperactivity. Its manifestations can extend far beyond these primary traits, often leading to misdiagnosis and misunderstanding. Learning about the intricate relationship between ADHD and these overlapping conditions is crucial for personal development, accurate identification, and effective intervention.
At first glance, the racing or restless mind of someone with ADHD resembles the anxious tendencies of an individual grappling with an anxiety disorder. The constant barrage of thoughts leading to difficulty falling asleep, maintaining focus can evoke a pervasive sense of worry and apprehension. Those with ADHD often find themselves consumed by a whirlwind of racing thoughts, as the mind attempts to anticipate potential pitfalls and over analyze situations of daily life. This chronic state of hyperarousal can heighten their susceptibility to stressors, further exacerbating their anxious tendencies.
The ADHD impersonation of Depression is a long time coming. The chronic struggles inherent in ADHD can wear down one’s mental well-being, decreasing the effectiveness of coping skills and paving the way for depression. The relentless battle to keep up with daily tasks, emotional burdens, and societal expectations can leave individuals feeling overwhelmed and disheartened. Ongoing weeks and years of continual feelings of inadequacy, and doubt accompanied by the inability to meet expectations, lead to a downward spiral of negative thoughts and emotions. The ADHD-related challenges that lead to the emotional burden of depression can create a formidable barrier to daily functioning and a negative outlook on what life has to offer.
If that’s not enough, emotional dysregulation is also a common trait imposed on individuals with ADHD. So common, one could argue, it should be part of the DSM-V diagnostic criteria for ADHD. As mood dysregulation is not diagnostically associated with ADHD it could be the reason symptoms of mood disorders, such as bipolar disorder or cyclothymia are seen as independent problems leading to misdiagnosis and ineffective treatment plans further blurring the lines between mental health conditions. Individuals with ADHD may experience intense emotional lability and rejection sensitivity, finding it a daily challenge to navigate the chaos of their internal landscapes.
These problems that stem from ADHD are often labeled as anxiety, depression, and mood dysregulation which highlights the importance of effective assessment and treatment planning. When using DSM-V checkbox-style diagnostic criteria, ADHD tends to be unrecognized, misdiagnosed, and ill-informed and ineffective treatment plans are implemented. Clinicians must adopt a more holistic understanding of ADHD and how it manifests across the entirety of their patient’s mental health, considering the cross-over of a multitude of symptoms.
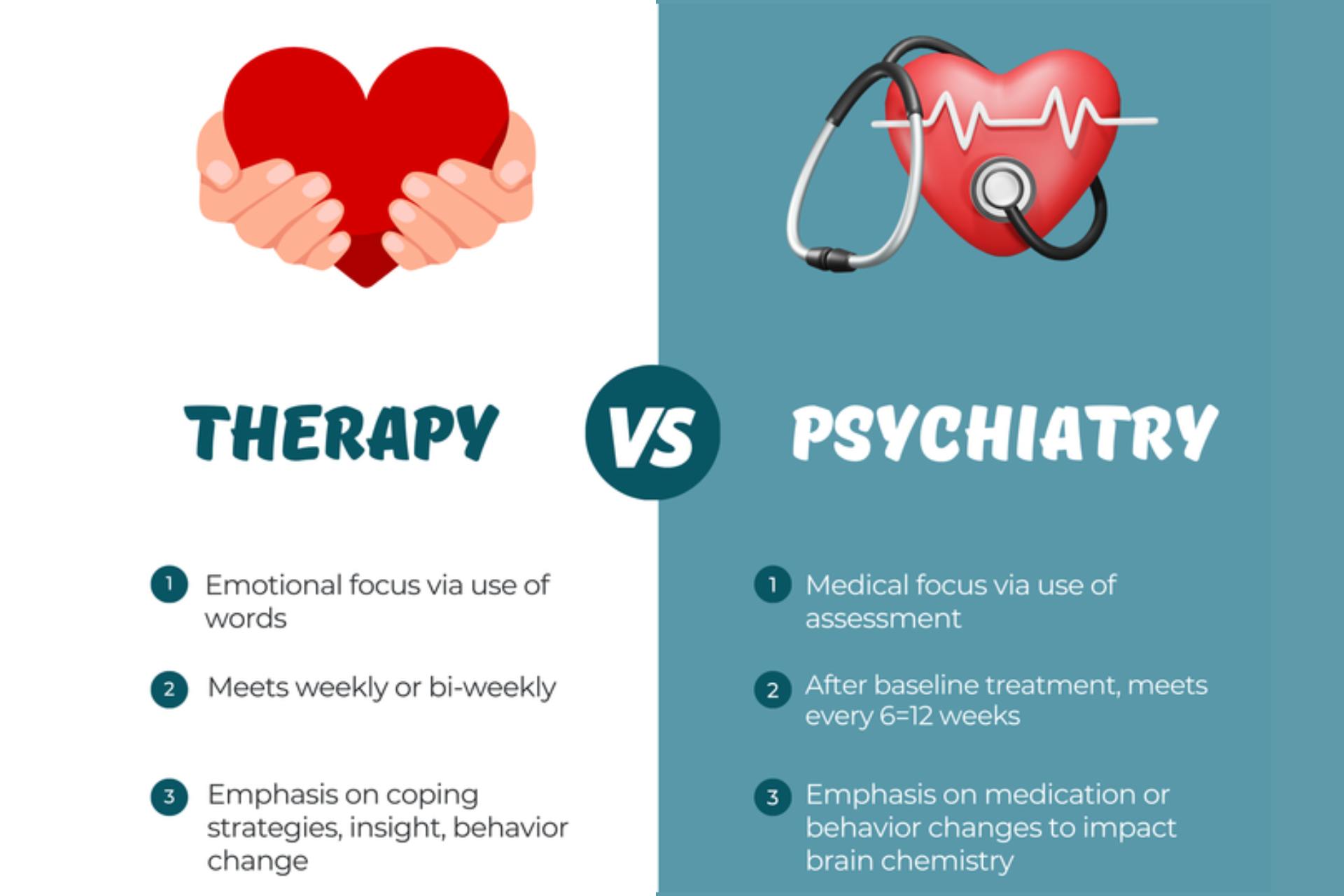
Medication management is often considered part of a comprehensive treatment plan for individuals with ADHD even in the presence of comorbid mental health problems. The approach to utilizing medication as tools varies widely between prescribers but in general should be seen as a tool to support ongoing executive functioning skill specific to ADHD which in concert will increase function. This functional increase can be used to implement and practice new skills and behavioral patterns, many of which can be maintained without medication.
In conclusion, ADHD is an underdiagnosed and misdiagnosed due to the symptoms that look and feel like anxiety, depression, and mood dysregulation. By recognizing the symptoms and understanding an individual’s expression of the problems, clinicians can provide more accurate treatments plans for individuals with ADHD. Through a collaborative and holistic approach to care, I would love the opportunity to get to know you and help create a specific treatment plan that brings about increased mental capacity. The decision to start something new or change directions is one that takes careful considerations.
Begin Where You Are
Dr. Tim Richardson | DNP, ARNP, PMHNP-BC
Resources
Riglin L, Leppert B, Dardani C, Thapar AK, Rice F, O’Donovan MC, Davey Smith G, Stergiakouli E, Tilling K, Thapar A. ADHD and depression: investigating a causal explanation. Psychol Med. 2021 Aug;51(11):1890-1897. doi: 10.1017/S0033291720000665. Epub 2020 Apr 6. PMID: 32249726; PMCID: PMC8381237.
D’Agati E, Curatolo P, Mazzone L. Comorbidity between ADHD and anxiety disorders across the lifespan. Int J Psychiatry Clin Pract. 2019 Nov;23(4):238-244. doi: 10.1080/13651501.2019.1628277. Epub 2019 Jun 24. PMID: 31232613.
Soler-Gutiérrez AM, Pérez-González JC, Mayas J. Evidence of emotion dysregulation as a core symptom of adult ADHD: A systematic review. PLoS One. 2023 Jan 6;18(1):e0280131. doi: 10.1371/journal.pone.0280131. PMID: 36608036; PMCID: PMC9821724.